
If you’re new to sleep apnea treatment, you’re most likely wondering where to start. What are the different machines? How are they similar and different from one another? And ultimately, you’re questioning which one is the best for you.
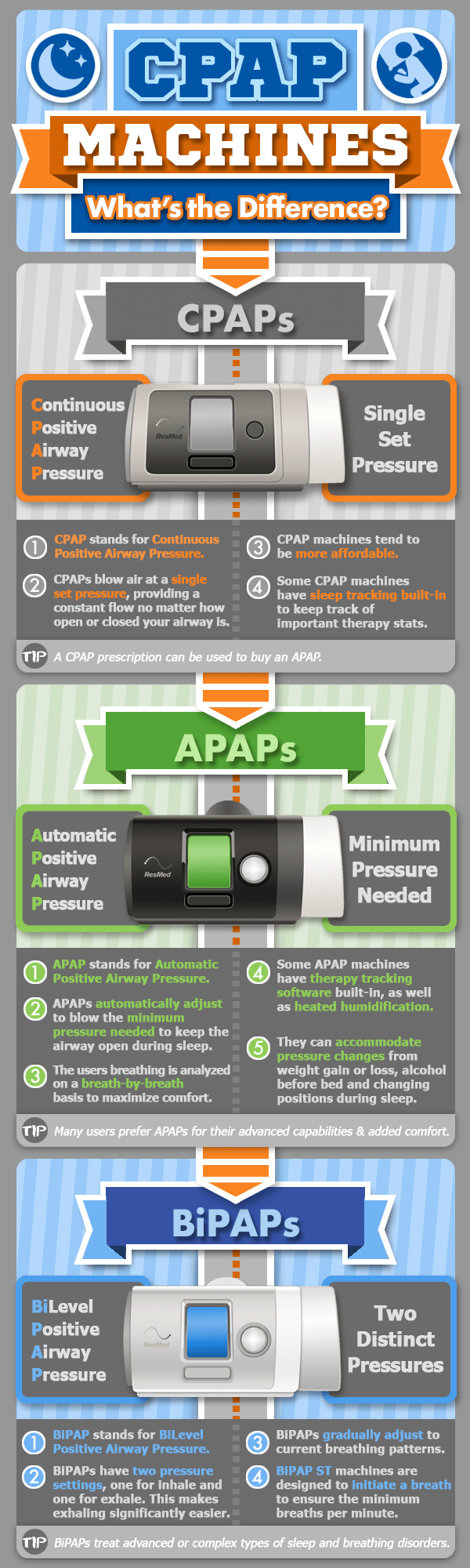
First things first—you’re most likely seeing the different terminology and acronyms for sleep apnea therapy machines. The terms that have been tossed around the most are likely continuous positive airway pressure (CPAP), bi-level positive airway pressure (BiPAP,) and automatic positive airway pressure (APAP.)
But, what do they all mean?
All three machines are forms of positive airway pressure therapy (PAP) and are designed for treating Obstructive Sleep Apnea (OSA). OSA is one of the three types of sleep apnea. All three acronyms describe machines that along with a CPAP mask and tubing provide a gentle flow of pressurized, filtered air to keep your airway open. These three machines keep obstructions from blocking your ability to breathe when you’re asleep.
Regardless of which machine you choose, your path to a better night’s sleep will start with a sleep study, which is either done in a specialized lab or as a home sleep study. Either study will help your doctor or sleep specialist determine which machine is right for you while also discovering your specific pressure setting.
Your pressure settings are measured in centimeters of water (cmH2O). Most CPAP and APAP machines can be set to anywhere between 4 to 20 cmH2O. BiPAP machines can be adjusted in a lower or higher pressure setting range since they are designed for those with severe OSA, central sleep apnea (CSA), and other serious respiratory disorders.
Three Main Types of Sleep Apnea Machines
- CPAP. After completing your sleep study, your physician may prescribe you a CPAP machine along with the exact air pressure setting you need to help you breathe while asleep. This air pressure is a constant flow set to the same pressure setting all night. You breathe in with the assistance of this pressure setting, and you exhale against this same pressure setting. CPAP machines are the most popular for treating OSA.
- APAP. An APAP machine is automated to work within a pre-set pressure range. An APAP machine automatically adjusts throughout the night to fit your specific pressure needs on a breath-by-breath basis. This makes APAP machines more comfortable.
- BiPAP. BiPAP stands for bi-level positive airway pressure. As the name implies, a BiPAP machine offers two levels of airway pressure: one for inhalation and another one for exhalation. BiPAP machines allow those with severe OSA to cycle air in and out of their lungs easier.
Why Choose CPAP Therapy?
Why CPAP over APAP or BiPAP?
CPAP machines have been around for over 40 years. CPAP machines were pioneered by an Australian doctor, Dr. Colin Sullivan, whose long-term research interests in the role of the upper respiratory airway in sudden infant death syndrome (SIDS) led him to discover that PAP therapy could also be used to treat sleep apnea.
This research and their ease of use make CPAP machines a safe and effective way to keep your airway open throughout the night, preventing apnea events.
If you have sleep apnea, you may have excess throat tissue that loses tone and relaxes while you sleep. The excess throat tissue falls backward and blocks your ability to breathe. Each one of these moments may cause you to gasp yourself awake to get a breath in. These are called apnea events.
CPAP machines can also treat Upper Airway Resistance Syndrome (UARS). UARS is a precursor to OSA. Instead of experiencing a full blockage, you will have a reduction in your air intake because your airway is crowded due to a buildup of loose tissue.
You may not gasp yourself awake due to a total loss of oxygen, but you will experience labored breathing, and your lungs will need to work harder to take in air as you sleep. Although you are breathing and taking in some oxygen, it may not be enough and sometimes your brain may wake you up to allow you to breathe more freely and consistently. If left unchecked, UARS will usually progress into OSA.
If you’re an otherwise healthy individual with no history of lung or respiratory disease and if you have been diagnosed with mild or moderate OSA, CPAP machines will likely be your first step when treating sleep apnea.
APAP: Advantages to Automated Pressure
Why might someone prefer to use, or need, an APAP machine over a CPAP or BiPAP machine? An APAP machine (sometimes referred to as an “automatic” or “autoset” machine) uses computer algorithms to determine what air pressure you require at any given moment while asleep, depending on variables such as your body position or how your breathing changes during the various sleep stages.
If you have sleep breathing patterns that vary over the course of the night, APAP therapy may be more comfortable for you. While most people with OSA do fine with a CPAP, others may get better results with an APAP because they report it feels more like natural breathing. You may prefer an APAP machine if:
- Your apnea events increase during rapid eye movement (REM) sleep and decrease during the other sleep stages. Some people need a higher air pressure during REM sleep only. If that high pressure remains high during the other sleep stages when you don’t really need it, then you may wake up due to discomfort. An APAP is capable of adjusting pressures accordingly.
- You toss and turn during sleep. If you spend part of the night on your back and part on your side, your snoring and apnea events may change depending on your sleeping position. You may need a higher inhalation pressure when you’re on your back as a result of gravity pulling the loose tissue downward toward the back of your throat.
- You sleep on your side. If you sleep on your side, which is one of the preferred sleeping positions for sleep apnea, your number of apnea events may decrease. The APAP can adjust the air pressure depending on your sleep position, so you don’t need to use the highest pressure setting at all times.
Some with sleep apnea also appreciate using an APAP machine because of its flexibility and comfort: a CPAP machine cannot function like an APAP machine but an APAP machine can be set to a single pressure setting and work like a CPAP. The adjusting air pressures based on your specific needs lead to a more comfortable night.
BiPAP: Why Is Bi-level Pressure Helpful?
First, it’s important to note that BiPAP is a trademarked brand name for Philips Respironics machines; however, many physicians and suppliers use the term as a catch-all for such machines. You may also see it referred to as BPAP, but both acronyms are different terms for the same therapy.
Why Would You Need Two Airway Pressure Settings?
BiPAP therapy is used when a lower exhalation setting is helpful if you have difficulty exhaling against the pressure setting you use to inhale. An example of when this might happen is if you have severe OSA and your inspiratory setting needs to be high in order to keep your airway open and exhaling against such a high setting may be difficult.
Over time, not being able to exhale carbon dioxide can be dangerous for your health as you are not inhaling enough oxygen. The CO2 can build up in your system, throwing off your blood gas levels and leading to severe health problems like organ damage. In the shorter term, having trouble exhaling may disturb your sleep and wake you up.
A doctor may prescribe a BiPAP rather than CPAP if you have breathing issues that may affect your ability to exhale against a higher air pressure. The conditions are:
- CSA (Central Sleep Apnea)
- Chronic Obstructive Pulmonary Disease (COPD)
- Overlap Syndrome
- Obesity Hypoventilation
Now that you have a better grip on what makes each machine stand out, the major similarities between APAP, BiPAP, and CPAP machines are that they all help to open your airway and facilitate breathing while you sleep, reducing the number of apnea events.
The main difference among them is how they do that.
While a CPAP machine is the standard therapy for most people with sleep apnea, BiPAP and APAP machines may offer greater comfort if you have variable breathing patterns or respiratory conditions that make exhaling against a higher pressure uncomfortable or need varying pressures throughout the night.
Remember that no machine is the best over the other—the right one is the one that will help you breathe easier at night to experience all the benefits of CPAP therapy, so you can get a restful night’s sleep. Because of this, we’ve created a detailed guide of the best CPAP machines to help you choose the right fit for your needs, so be sure to read that next!



3 Responses
Thank you for sharing.
I just received the Phillips Dream Station and used it for the first time last night and it was great. I have been using a CPAP for over 20 years and they have really gotten better, and the price here was great too. It does surprise me that the mask here in proportion to the machines are so high? Had originally purchased this for my step-father, who broke his and I had let him use mine because I still had a older one set for me. I think that I will let him use mine until next year when he is eligible for a new one and then purchase him one of these as well.
That was an excellent explanation, thank you so much. I get it now.